Abstract
Objectives: We evaluated outcomes in couples treated for infertility with natural procreative technology (NaProTechnology, NPT), a systematic medical approach for optimizing physiologic conditions for conception in vivo, from an Irish general practice.
Methods: All couples receiving treatment from 2 NPT-trained family physicians between February 1998 and January 2002 were studied. The main outcome was live birth, and secondary outcomes included conceptions and multiple births. Crude proportions and adjusted life-table proportions were calculated per 100 couples.
Results: A total of 1239 couples had an initial consult for NPT, of which 1072 had been trying for at least a year to conceive and initiated treatment. The average female age was 35.8 years, the mean duration of attempting to conceive was 5.6 years, 24% had a prior birth, and 33% had previously attempted treatment with assisted reproductive technology (ART). All couples were taught to identify the fertile days of the menstrual cycle with the Creighton Model FertilityCare System, and most received additional medical treatment, including clomiphene (75%). In life-table analysis, the cumulative proportion of first live births for those completing up to 24 months of NPT treatment was 52.8 per 100 couples. The crude proportion was 25.5. Younger couples and couples without previous ART attempts had higher rates of live birth. Among live births, there were 4.6% twin births.
Conclusion: NPT provided by trained general practitioners had live birth rates comparable to cohort studies of more invasive treatments, including ART. Further studies are warranted to compare NPT directly to other treatments.
Infertility is a common problem; one in every 7 couples hoping to have a baby experiences difficulties achieving or maintaining pregnancy serious enough to seek medical intervention.1 Infertility is a chronic problem that involves both women and men, has major psychosocial ramifications, and usually requires addressing multiple issues, including comorbid medical conditions and lifestyle, all key elements of primary care practice. However, treatments for infertility are largely provided by physicians trained in subspecialties, including artificial insemination, ovulation induction, and hormonal support of the menstrual cycle.1,2 The increasing shift of treatment toward assisted reproductive technologies (ART), including in vitro fertilization and intracytoplasmic sperm injection, has removed infertility treatment further from the realm of the generalist or family physician.1,3
ART is expensive, invasive, and involves some risk to women. These include risks of the medical and surgical procedures to retrieve oocytes,4 including ovarian hyperstimulation syndrome.5 There are also concerns about short- and long-term outcomes for the offspring.6–9 The most prominent concerns relate to the incidence of multiple pregnancies with ART treatment and the subsequent perinatal complications, including low birth weight and prematurity.10–12 Increasing the availability of integrated primary methods for infertility treatment that can be effectively provided by a trained generalist physician with low risk to women and offspring would potentially improve access to care for couples dealing with infertility.
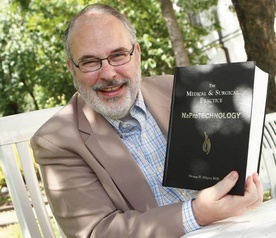
Natural procreative technology (NaProTechnology, NPT) is an integrated and systematic approach to infertility that is suitable for primary care settings. It is based on a detailed study of events that occur during ovulation and throughout the menstrual cycle.13,14 Abnormalities of the reproductive cycle are identified and corrected to the extent possible.15–18 Patients receive thorough education about their fertility and are taught to monitor biomarkers of their own fertility cycles. In the process, they become equal partners in their own evaluation and treatment.
A standardized NPT investigation usually results in the diagnosis of one or more abnormalities of reproductive function that are associated with infertility. Abnormalities commonly identified include decreased production of estrogenic cervical mucus, intermenstrual bleeding or spotting, short or variable luteal phases, and suboptimal levels of the ovarian hormones estrogen and progesterone.19 The physician trained in NPT then determines a course of treatment that aims to correct the underlying abnormality, with the goal of optimizing physiologic conditions for conception in vivo. Common interventions include induction or stimulation of ovulation20; medications to enhance cervical mucus production, including vitamin B6, guaifenesin, or one of several antibiotics21,22; and hormonal supplementation in the luteal phase.23 Doses of all medications are adjusted according to the response of biomarkers and serum levels of estrogen and progesterone measured in the midluteal phase.13,17 Concurrently, couples use their awareness of ovulation biomarkers to time acts of intercourse to maximize chances of conception.24 Ongoing evaluation and support during pregnancy often includes supplementation with human-identical progesterone, based on periodic measurement of progesterone levels, in an effort to reduce the risk of adverse pregnancy outcomes.25–28
Outcomes for NPT have been published previously for a cohort of infertility patients in a specialty practice at its place of development (Creighton University).29 This study was undertaken to assess the outcomes of NPT as applied by trained generalist physicians in Galway, Ireland. Although NPT has been developed with both medical and surgical protocols, this study evaluates the medical protocols. We focused on the clinically relevant outcomes of live birth and multiple births.
Pełny tekst wersja pdf:
Outcomes From Treatment of Infertility With Natural Procreative Technology in an Irish General Practice_2008
Wersja online:
Journal of the American Board of Family Medicine: Outcomes From Treatment of Infertility With Natural Procreative Technology in an Irish General Practice